Hormones. It’s easy to blame them for everything, from mood swings to food cravings to those extra pounds that don’t quite make sense. While weight fluctuation can be totally normal and healthy, truly unexplained weight gain can point to a hormone imbalance and might be your body’s way of asking for extra help.
If weight loss is a goal, it’s essential to understand your hormones, not blame them!
Progesterone is one of two major menstrual cycle sex hormones that play an interesting role in regulating body weight (among its lengthy list of distinguished accomplishments). Supporting our body’s progesterone production and understanding how it changes throughout life can help us maintain a healthy weight.
What Is Progesterone?
Progesterone is a sex hormone produced in the ovaries following ovulation. It peaks during the luteal phase of the menstrual cycle and works to prepare the body for the possibility of a pregnancy.
It also sticks around through gestation to maintain a healthy pregnancy.
What else does it do? Progesterone also plays a role in protecting our brains, bones, metabolism, mood, libido, and thyroid hormone levels.
Progesterone and estrogen (another important sex hormone) both decrease as a woman enters menopause.
Progesterone and Weight
One of the critical ways that progesterone can affect weight is through its interaction with estrogen. When hormone levels are ideal, progesterone and estrogen form a natural balance in our body, regulating the other’s effects. In some tissues, progesterone limits the function of estrogen receptors, helping control the impact of estrogen on those cells.
While estrogen promotes storing energy as fat (particularly in the breasts and hips), progesterone allows our bodies to metabolize that fat, burning it for energy. Estrogen (and aldosterone, an adrenal hormone) help us retain salt and water, while progesterone is a natural diuretic, allowing water loss and decreasing swelling.
In each of these balances, progesterone doesn’t cause weight loss. Instead, it helps reduce the effects other hormones have on weight gain. When progesterone and estrogen work together, all these factors balance out to promote healthy, fertile weight regulation.
When progesterone levels drop too low, these checks and balances go haywire, and weight gain can sneak in. Our estrogen does SO MANY awesome things for our bodies, but without ample progesterone to rein it in, we can experience something called estrogen dominance. The PMS hits hard, we’re bloated, crampy, grumpy, and our thighs are holding tight to weight that wasn’t there before.
If you suspect your hormones could use a tune-up, sign up for my Hormone Starter Kit with 7-day Meal Plan to give your hormones what they need to find balance.
Reasons Progesterone Can Cause Weight Gain
Supporting healthy progesterone levels – not too high, not too low– is key to supporting healthy metabolism
Progesterone and Insulin Resistance
Both too much and too little progesterone can impair your body’s blood sugar regulation.
During a healthy pregnancy, progesterone and other hormone changes decrease the mother’s sensitivity to insulin. This insulin resistance helps elevate blood sugar levels and ensures that your body delivers enough nutrients to the growing fetus.
Without a fetus to feed, high progesterone (and low relative estrogen) can also cause “hyperinsulinemia,” meaning it increases the amount of insulin present in the blood. Too much insulin could cause your body to convert even more blood sugar for storage as fat. This is why you may have more food cravings, feel more hungry, and have a more difficult time losing weight during the luteal phase of your cycle when progesterone is highest.
However, low progesterone can also mess with your insulin response, another reason to work closely with a doctor to confirm any hormonal hunches. Low progesterone is linked to PCOS, which is associated with insulin resistance. Excess estrogen can lead to insulin resistance as well!
PCOS is complex, but it is important to clarify that weight loss won’t cure PCOS and your weight gain didn’t cause it. It’s important to monitor weight to understand the hormonal and metabolic influence, but too often doctors hyperfocus on weight and often shame women about it. PCOS causes weight gain. Addressing the factors of PCOS is what is important.
@drjolenebrighten Have you heard that weight gain causes #pcos ? #pcosweightloss #drjolenebrighten #weightlossjourney
♬ Elastic – Joey Purp
Thyroid Hormone and Body Composition
Thyroid hormone is a critical factor in metabolism, especially when it comes to burning fat. When progesterone levels are too low compared to estrogen, the body produces too much of a protein called Thyroid Binding Globulin (TBG). This protein prevents the normal functioning of thyroid hormones.
This can be a confusing source of weight gain, as the thyroid gland may still produce the proper amount of thyroid hormone, so thyroid tests may appear normal. However, since low progesterone can prevent our body from using those thyroid hormones, we can still experience symptoms of hypothyroidism, such as weight gain.
Hormone Imbalance and Increased Appetite
For many of us, it’s absolutely no surprise that hormones affect our appetite. (Just ask that empty carton of ice cream.)
Progesterone and estrogen also have opposite effects on hunger; however, excess progesterone can drive weight gain. Higher estrogen levels reduce appetite while also reducing the amount of ghrelin (the hunger hormone) that our brains receive. Progesterone, on the other hand, stimulates our appetite.
If you feel like quitting hormonal birth control or hitting menopause had a noticeable effect on your cravings, this could be a clue to look closer at your hormones.
What Causes Low Progesterone?
Because the ovaries create progesterone after releasing an egg, a woman who is not ovulating will likely experience progesterone deficiency symptoms. Missing cycles can result from hormonal birth control, hypothalamic amenorrhea, PCOS, over-exertion, or post-birth control syndrome.
Progesterone levels can also decrease in response to menopause, stress, hypothyroidism, PCOS, overproduction of prolactin. Even with adequate progesterone, elevated estrogen levels can still throw off that balanced ratio, leading to symptoms of too much estrogen, not enough progesterone.
Low progesterone symptoms can also include:
- Insomnia or sleep disturbance
- Low libido
- Mood changes, anxiety and irritability
- Breast tenderness
- Headaches and migraines
- Weight gain
- Irregular menstrual cycle
- Short cycles
- Mid-cycle spotting
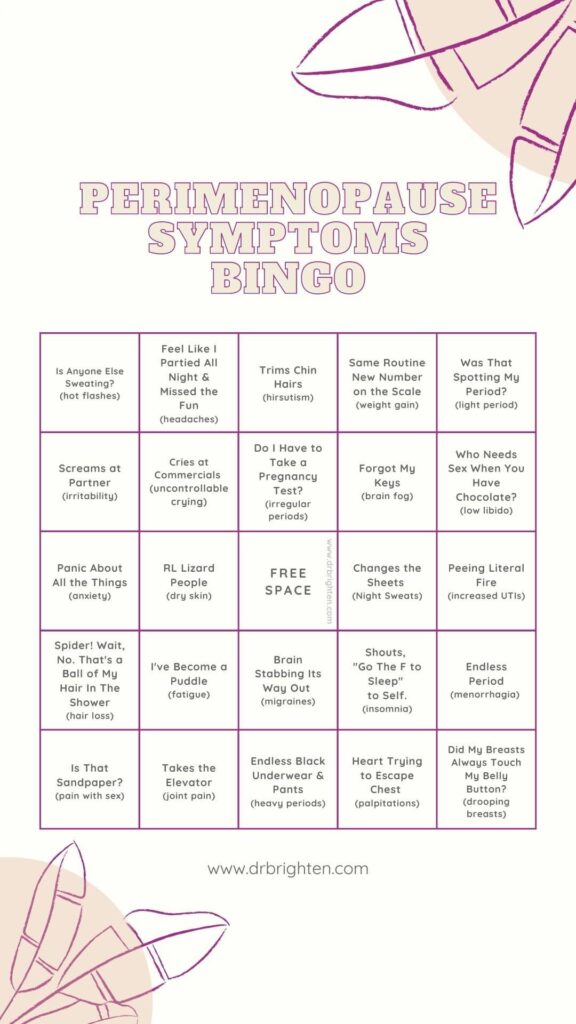
How Progesterone Can Cause Weight Gain During Menopause
For many women, weight gain is a common symptom of perimenopause and menopause. Dramatic changes in hormone levels mean our bodies might react differently to the same diets and routines we’ve kept for years.
In some cases, weight gain during menopause can be linked to estrogen dominance. Wait – aren’t we producing less estrogen? It might seem backward to think of estrogen dominance after menopause, but progesterone production that drops off faster than estrogen levels can again throw off that ratio.
Many factors impact our hormones and our weight during perimenopause and menopause, so it’s essential to work with a provider to identify the best course for your goals. If your progesterone levels are out of whack, your doctor may recommend a bioidentical hormone replacement therapy (BHRT) such as progesterone cream. If used correctly, supplementing your body with bio-identical progesterone can help combat the effects of estrogen dominance, including weight gain.
Is Weight Gain A Side Effect Of Progesterone?
Weight gain can also be a concern for women considering BHRT progesterone therapy, and the confusion of progesterone with scarier synthetic options certainly doesn’t help.
Many studies used to determine progesterone’s side effects studied progestin, a synthetic progesterone replacement. Progestin is not the same as progesterone, and your body definitely knows the difference. Progestins, like those found in combination birth control pills or synthetic hormone therapy, can cause water retention and bloat, unlike natural progesterone. On top of this, taking progestins can actually shut down our bodies’ natural production of progesterone, which can push us further towards estrogen dominance and unwanted weight gain.
If you need to supplement your progesterone production, talk to your doctor about the options to find what will work best for you, and make sure they know the difference. I’ve found clinically that the majority of my patients do better with a bioidentical progesterone opposed to using hormonal birth control for perimenopause and menopausal symptoms.
Can Progesterone Cause Weight Loss?
Progesterone therapy can be useful for weight loss if progesterone levels are unbalanced. Identifying triggers for weight changes can be hugely tricky, and it’s essential to work with a qualified practitioner to understand our bodies’ needs fully. Hormone therapy should never be used as a quick fix for weight loss, and its misuse can cause serious problems.
Remember, we’re working to understand our hormones, not blame them. Our hormones are a beautiful, complex system that cares for us in ways we’re still learning to understand.
Weight Changes as a Signal (Not a Flaw)
Understanding progesterone and the progesterone-estrogen balance is key to understanding our bodies’ changes, especially as we age. While frustrating, unexplained weight gain can be a critical message from your body, cluing you in to changes that need support.
Following these clues and listening to your body are the best way to get the vibrant, healthy hormones you need. Read more here to learn about progesterone deficiency’s underlying causes and 9 ways to boost your progesterone production naturally.
Read next: 9 Ways to Increase Progesterone & Boost Fertility
Unexplained weight gain or loss is generally a symptom of something else going on in your body. It’s my intention that this article will help you understand how your hormones may be at play and help you have a more informed discussion with your provider.
Your weight is one data point that isn’t that useful on its own in determining health.
As a gentle reminder, weight loss isn’t a cure all for every concern you may have—even if your doctor says it is.
@drjolenebrighten The cringe. #pcos #womenshealth #drjolenebrighten #periodproblems
♬ Somebody to love Basstrologe Bootleg – mthekyng
@drjolenebrighten Have you heard that weight gain causes #pcos ? #pcosweightloss #drjolenebrighten #weightlossjourney
♬ Elastic – Joey Purp