Hashimoto’s is an autoimmune condition that primarily affects the thyroid gland and has been correlated with autism in the offspring of mothers with the condition. Without intervention, the result is immune destruction to the mother’s thyroid, often with a need for medication.
There is somewhat of a “myth” in mainstream medicine that leads some doctors to the conclusion that once the thyroid is completely destroyed and proper medication dosage has been achieved the disease is managed, without concern for further organ involvement.
Unfortunately, there are many sequelae that accompany Hashimoto’s, including the risk of developing multiple other autoimmune diseases. In fact, once you have one autoimmune condition, it is highly likely you will develop another.
Several studies have identified correlations between mothers with autoimmune disease and an increase incidence of autism in their offspring. Conditions such as Hashimoto’s, type 1 diabetes, inflammatory bowel disease and celiac disease have all be correlated with an increased risk of autism.
In a recent study, infants of mothers who tested positive for Anti-TPO antibodies (the primary antibodies found in Hashimoto’s) during pregnancy saw an increased odds of autism by nearly 80%. I don’t know about you, but to me, 80% is a reason to pause and reconsider how we are approaching autoimmunity, especially in our mothers.
Register for the free upcoming Autism Intensive Summit.
In a recent review regarding autoimmunity and thyroid disease, it was concluded that autoimmunity developed during pregnancy and thyroid disease were both associated with autism risk in baby. Furthermore, they concluded that mom’s autoimmune disease is likely an independent risk factor in the development of autism in their child, with an estimated 30% increased risk.
What role does Mom’s autoimmunity have in autism development?
There are two main theories as to how maternal autoimmunity influences the development of autism in her baby.
Immune Modification: The dysfunction in mom’s immune system during fetal development is thought to alter baby’s immune system at the genetic level.
Fetal Brain Development: Mom’s immune mediators, including cytokines, T cells and autoanitbodies pass through the placenta into baby’s brain leading to activation of microglia, the main immune system defense of the brain. The activation of microglial cells leads to inflammation in baby’s brain, which inhibits proper development.
Much more research and understanding is needed to fully grasp the role of mom’s autoimmunity during pregnancy and the long term affects on fetal brain development. But I understand that reading this may feel a little overwhelming or even a bit defeating if you currently have an autoimmune disease. But there are many steps you can take to bring your immune system back into balance prior to conception.
In a recent interview for the Autism Intensive, I shared approaches to preconception that improve both the health of mom and baby. You can register to watch the interview here.
Autoimmune Management as Part of Preconception Care
As a Functional Medicine and Naturopathic Physician, I take a holistic approach to caring for my patients. Autoimmune diseases, like Hashimoto’s can make conception much more difficult, increases the risk of miscarriage and other complications in pregnancy, and has been correlated with higher incidences of postpartum complications, like depression.
These 7 Steps are important for all women wishing to conceive, bust especially those with Hashimoto’s.
Get Tested: Work with a qualified healthcare practitioner to determine appropriate testing for you. You should have a complete thyroid panel prior to conception, as well as testing to determine your gut health. Because many Hashimoto’s patients have nutrient deficiencies, screening for these is also important. Download my list of pre-pregnancy lab testing for Hashimoto’s.
Vitamin D: Check your levels and supplement appropriately. Low vitamin D has been associated with chronic disease and has a large role to play in balancing your immune system.
Eat Your Omegas: Omega-3 fatty acids, like those found in cold water fish, reduce inflammation, improve brain health and are beneficial in immune system regulation. Don’t like fish? You can find these omega-3 fatty acids in fish oil supplements. Aim for 1,000-3,000 total omega-3 daily and always be sure to purchase from a company that uses third party testing and screens for heavy metals.
Remove Food Sensitivities: At minimum, I tell my patients to ditch gluten. An elimination diet is one of the best ways to determine if you have other food sensitivities. Food sensitivities can perpetuate autoantibodies in your system.
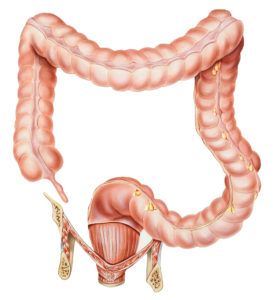
Fix Your Gut: It houses the majority of your immune system. If you have an immune problem, you need to look to your gut to fix it. In my practice I’ve seen countless patients significantly improve their autoimmune condition after discovering and treating their SIBO, chronic yeast, bacterial overgrowth, parasites and/or intestinal permeability. And it is worth noting that what your grow in your gut will have a direct impact on baby’s.
Manage Your Stress: Stress is a constant in our lives and can drive your autoimmunity full steam ahead. The good news is that how your respond to and manage your stress can have a significant impact on your immune system and your entire well being.
Preconception Detox: Daily detoxification is a must for your health and baby’s. I find many of my autoimmune patients have either issues with the way their body eliminates waste or have a build up of toxins, including heavy metals and endocrine disruptors, in their system. Detoxing a good 6-12 months prior to conception can alleviate your symptoms, decrease your autoimmunity, improve thyroid function and make conception so much easier.
I’m a strong advocate for the management of autoimmunity prior to conception and as such, I have put together a comprehensive program that focuses on preconception care for women with Hashimoto’s. As a mother and a doctor with Hashimoto’s, it is my mission to help women with Hashimoto’s have the most optimal pregnancy outcomes.
Join my mailing list now to receive exclusive offers and special pricing on my Hashimoto’s Preconception Program opening in 2016.
And don’t forget to sign up for the Free Autism Intensive airing in January 2016.